Understanding and treating disease
In 2006, a discovery opened up a new world of possibility for treating diseases. For the first time, researchers created stem cells without using embryos. Adult skin cells were reprogrammed into induced pluripotent stem cells, or iPSCs, that could differentiate into specialized cells for use in almost any part of the body — from the liver to the heart or brain, and everywhere in between. Areas of the body damaged by disease could be made healthy again.
But after more than a decade of research on iPSCs, the process of creating them is still incredibly inefficient. “We have been puzzled that after 10 years of intense research in that direction, the efficiency of iPSC reprogramming is still only about 0.1 percent,” says Associate Professor Domitilla Del Vecchio. “It’s not really at the point that you can use it for clinical purposes.”
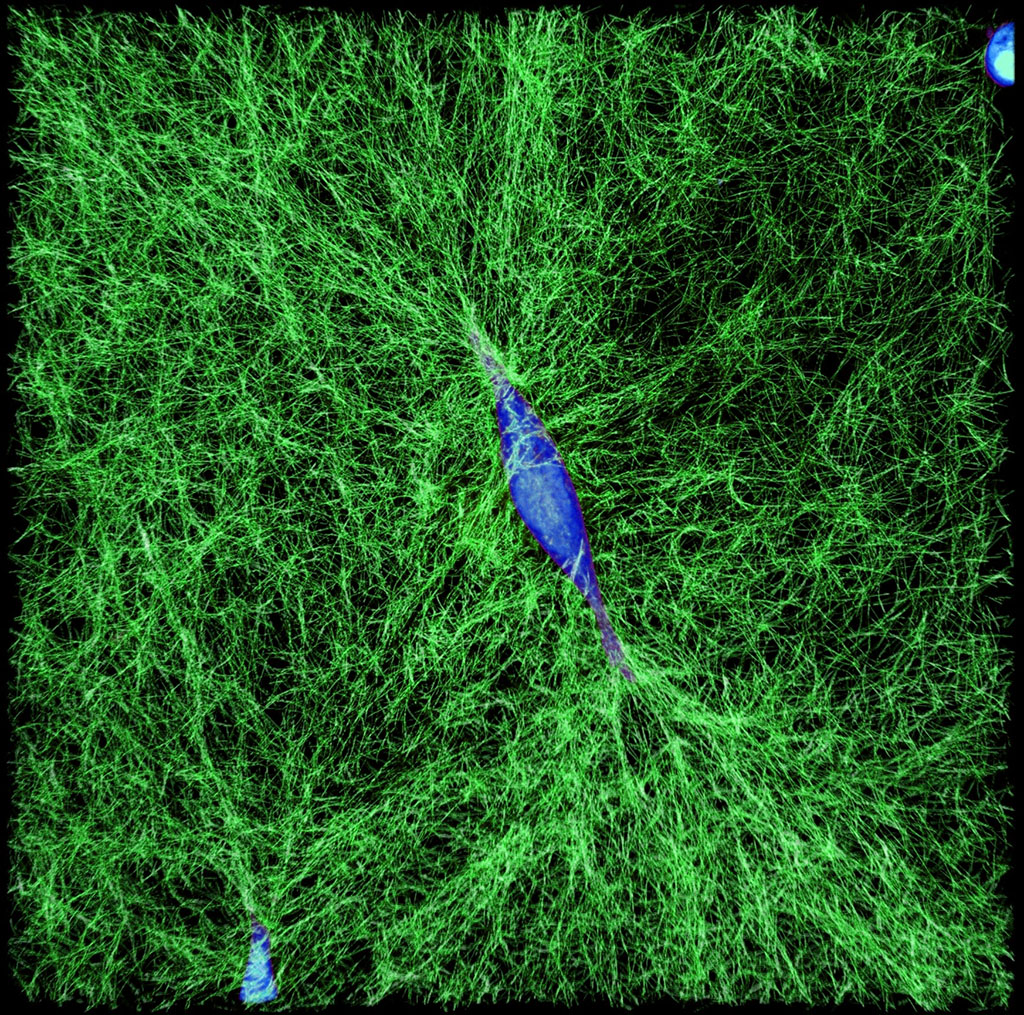
Del Vecchio and her colleagues are hoping to change that. Currently, researchers develop iPSCs by delivering synthetic DNA to the nucleus of a somatic cell, such as a skin cell. This synthetic DNA produces high levels of select proteins — known as transcription factors — with the aim of “pushing” the somatic cell to reprogram into a stem cell. But overloading a cell with such a high level of transcription factors leads to a highly inefficient process. “If you have a mechanical system, such as a car or a robotic manipulator, and you give it an arbitrary push, you should not expect that the system will end up exactly in the configuration you want,” says Del Vecchio.
To fix this problem, Del Vecchio and her team are adding accelerators and brakes to the process. Using mathematical analysis, they can demonstrate that with an appropriate balance the pluripotent stem cell state can be reached. With the help of small molecules, the synthetic DNA delivered via a virus can produce tunable levels of transcription factors based on a target configuration. This method — called a synthetic genetic feedback controller — can be used to steer the concentration of transcription factors in the cell to the point at which it can become a stem cell.
The applications of Del Vecchio’s work may have far-reaching implications for the way diseases are treated. Researchers could quickly create healthy heart cells for patients with a heart condition or beta cells for diabetic patients.
Del Vecchio’s eyes light up when discussing the possibilities. “It’s clearly high risk,” she admits. “But we want to proceed in this direction because if it works, it will be highly impactful for society and hence extremely rewarding for us.”
Giving doctors the ability to quickly create stem cells could change the way many diseases are treated. The research Del Vecchio’s team is conducting represents just one example of how mechanical engineering researchers across a diverse range of specialties are developing new and innovative ways to deepen our understanding of disease and unlock new therapies to treat it.
Diagnosing disease
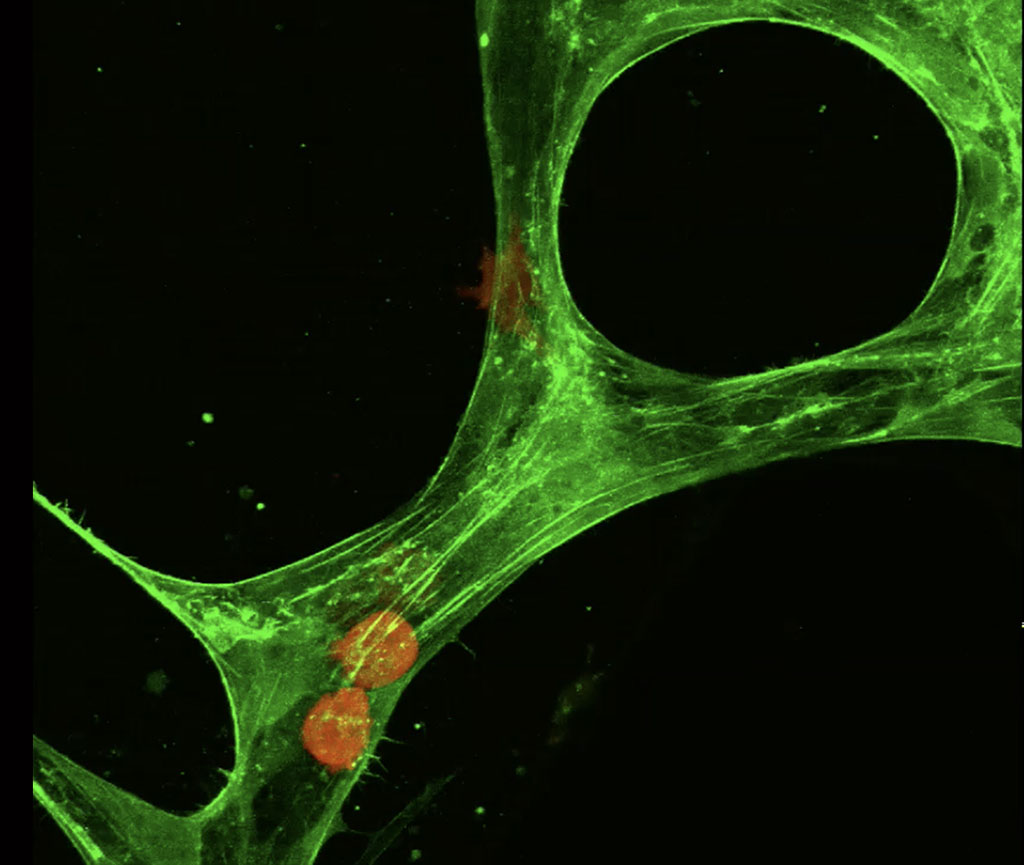
Understanding disease starts with the cell. Assistant Professor Ming Guo, who serves as the d’Arbeloff Career Development Professor, is interested in decoding the differences between the mechanical properties of a healthy cell and a diseased cell as a way to develop a diagnostic tool. “Just by looking at a healthy cell compared to a diseased cell, you can tell that they’re different mechanically,” says Guo.
Stiffness in particular is a key trait in distinguishing what kind of disease a cell has — for example cancer cells have been shown to be soft while asthma cells are often stiff. Currently, this information is probed by contact-only methods such as atomic force microscopes or optical tweezers, which use either a mechanical tip or a focused laser beam on a patient’s tissue to measure cell properties. Guo and his colleagues have now developed a safer, less invasive method of analyzing the mechanics of a cell to help formulate a diagnosis by simply taking a small sample of cells and watching them using a standard optical microscope.
“We came up with the method by simply observing the movement of organelles in the cell,” says Guo. The team took videos of cells under a microscope. They tracked the movements of individual organelles or particles within the cell at frequencies of 10 frames per second and higher. Then, by plugging the value of these movements into a generalized form of the Stokes-Einstein equation, they were able to calculate the exact stiffness of a cell.
“We found that high frequency fluctuation can help us gauge cell stiffness and understand its mechanics,” says Guo. Understanding these mechanical properties can help doctors diagnose diseases on the spot. Guo has begun collaborating with doctors at Massachusetts General Hospital on applying this method to cancer and asthma cells. The hope is that doctors and researchers can test drug efficacy by measuring a cell’s mechanics before and after treatment.
Tracking disease
While improving diagnostic methods could help catch a disease early, tracking how diseases grow could be key to developing new therapeutic interventions. Roger Kamm, the Cecil and Ida Green Distinguished Professor, and his lab use a device that’s roughly the size of a quarter to track tumor cells as they leave the vascular network and eventually grow into tumors. These tiny microfluidic devices can help us understand how cancer metastasizes.
“We’ve developed a 3-D vascularized network in which we can track cancer cells inside a capillary,” says Kamm. “It’s about understanding how cell populations interact. We can watch the tumor cells escape from the vessel to invade the surrounding tissue.”
The microfluidic device consists of two media channels on either side with 3-D hydrogel in the center. The gel is seeded with endothelial cells that form capillaries where the tumor cells are introduced. From there, Kamm and his team use microscopic imaging to watch every single movement the tumor cell makes. From intravasation — when a cancer cell enters the bloodstream — to extravasation — when a tumor cell leaves the blood stream and becomes metastatic — the cell’s path is studied with painstaking precision.
“Using microfluidics, we can follow this process over time,” explains Kamm. “After the cell enters the metastatic organ, we can see how a single tumor cell starts to multiply over days and how it begins to form a metastatic tumor.”
Microfluidic devices allow Kamm to analyze the forces that inform the cancer cell’s behavior. Understanding whether tumor cells push or pull when they leave the capillary and the force interactions between endothelial cells and tumor cells represent potential therapeutic targets for preventing or minimizing metastasis.
“We can look at all these different tumor cell lines, treat the different cells, and see how that affects the rate at which the tumor cells escape from the vasculature and grow,” says Kamm. This knowledge could open up new opportunities in treating cancer and even developing new immunotherapies.
Treating disease
Armed with more knowledge of how diseases grow and spread, researchers are better able to develop new ways to treat, and in some cases cure, disease. Among them is Assistant Professor Ellen Roche, who is taking a unique dual approach to treating heart disease using both mechanical and biological therapies.
“The idea is to mechanically assist the heart,” says Roche, who also serves as Helmholtz Career Development Professor at MIT’s Institute for Medical Engineering and Science. “Rather than take over its function we just assist and augment it using a biomimetic approach.”
Roche uses new techniques like soft robotics to develop devices that mimic both the tissue properties and the motion of the heart. One such device is a sleeve that wraps around the heart to assist with pumping. Soft robots like this sleeve use elastomeric materials and fluidic actuation to mimic an organ’s movement. “By smartly designing simple fluidics channels and reinforcing soft materials in just the right way, you can achieve very complex motion with just elastomeric changes, and pressurized air or water,” says Roche.
While working on mechanical therapies to treat things like congenital heart disease and heart attacks, Roche is also looking at how biological therapies can help in treating these diseases. She and her team are developing smart devices that provide localized drug delivery instead of systemic drug delivery.
“One of my main goals is to combine these mechanical and biological therapies and see how they interplay with each other,” says Roche. Understanding how these different therapies interact could help determine the best timing sequence for maximum efficacy. With the help of collaborators in the cardiac surgery group at Boston Children’s Hospital, Roche is creating and testing models for these therapies. “We really want to see if we can treat disease and recover function using polytherapy rather than just a mechanical or biological approach.”
Rehabilitation from disease
In instances when disease is not detected or treated in time, researchers are developing tools that assist in the recovery process. From optimizing the design of prosthetic feet or building cheaper wheelchairs, mechanical engineers are finding ways to improve the quality of life for those living with the aftermath of disease. This work also includes tools and devices that can be used in physical rehabilitation. One such tool is the MIT-MANUS — a robot developed by Professor Neville Hogan to help stroke victims recover and regain mobility.
“They say no two snowflakes are alike, well no two stroke patients are alike either,” says Hogan. “That makes the problem spectacularly complicated.” Hogan has collaborated with neurologists and neuroscientists on understanding the process of recovery and basic motor control in the brain. He used this knowledge to develop robots that interact with stroke patients and help them regain control of their movements.
MIT-MANUS was originally designed to help restore motor function in stroke patients’ shoulders and elbows. Patients strap their forearm into a brace attached to a robotic arm and grasp onto a controller connected to a video screen. On the screen, a video game provides patients with prompts to move their arm and wrist. If the patient is unable to fully move their arm on their own, MIT-MANUS provides guidance and assists their movements. The robot then tracks and stores this data for physical therapists and specialists to analyze.
“In clinical trials of MIT-MANUS we found that there was a reduction of impairment in joints exercised through use of the robot,” says Hogan. Over the years the scope of this robot-aided therapy for stroke victims has grown beyond hands and arms. Hogan and his collaborators have put together a robotic gym that helps deliver localized therapy to various limbs and joints throughout the body.
Whether it’s constructing large robots like the MIT-MANUS to help rehabilitate stroke victims, tracking the miniscule movements of organelles in the cell, or using genetic circuits to create stem cells, mechanical engineers are shaping both our fundamental understanding of disease and the way in which doctors approach treatments and therapies.