3 Questions: Peko Hosoi on the data-driven reasoning behind MIT’s Covid-19 policies for the fall
As students, faculty, and staff prepare for a full return to the MIT campus in the weeks ahead, procedures for entering buildings, navigating classrooms and labs, and interacting with friends and colleagues will likely take some getting used to.
The Institute recently reinforced its policies for indoor masking and has also continued to require regular testing for people who live, work, or study on campus — procedures that apply to both vaccinated and unvaccinated individuals. Vaccination is required for all students, faculty, and staff on campus unless a medical or religious exemption is granted.
These and other policies adopted by MIT to control the spread of Covid-19 have been informed by modeling efforts from a volunteer group of MIT faculty, students, and postdocs. The collaboration, dubbed Isolat, was co-founded by Anette “Peko” Hosoi, the Neil and Jane Pappalardo Professor of Mechanical Engineering and associate dean in the School of Engineering.
The group, which is organized through MIT’s Institute for Data, Systems, and Society (IDSS), has run numerous models to show how measures such as mask wearing, testing, ventilation, and quarantining could affect Covid-19’s spread. These models have helped to shape MIT’s Covid-19 policies throughout the pandemic, including its procedures for returning to campus this fall.
Hosoi spoke with MIT News about the data-backed reasoning behind some of these procedures, including indoor masking and regular testing, and how a “generous community” will help MIT safely weather the virus and its variants.
Q: Take us through how you have been modeling Covid-19 and its variants, in regard to helping MIT shape its Covid policies. What’s the approach you’ve taken, and why?
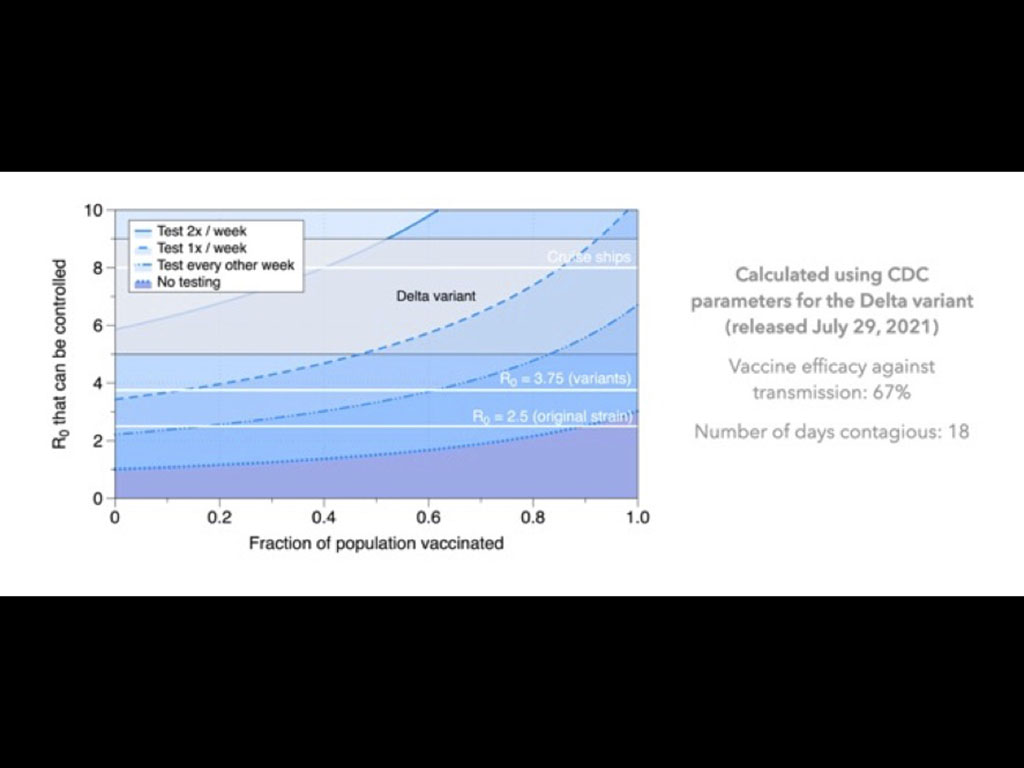
A: The approach we’re taking uses a simple counting exercise developed in IDSS to estimate the balance of testing, masking, and vaccination that is required to keep the virus in check. The underlying objective is to find infected people faster, on average, than they can infect others, which is captured in a simple algebraic expression. Our objective can be accomplished either by speeding up the rate of finding infected people (i.e. increasing testing frequency) or slowing down the rate of infection (i.e. increasing masking and vaccination) or by a combination of both. To give you a sense of the numbers, balances for different levels of testing are shown in the chart below for a vaccine efficacy of 67 percent and a contagious period of 18 days (which are the CDC’s latest parameters for the Delta variant).
The vertical axis shows the now-famous reproduction number R0, i.e. the average number of people that one infected person will infect throughout the course of their illness. These R0 are averages for the population, and in specific circumstances the spreading could be more than that.
Each blue line represents a different testing frequency: Below the line, the virus is controlled; above the line, it spreads. For example, the dotted blue line shows the boundary if we rely solely on vaccination with no testing. In that case, even if everyone is vaccinated, we can only control up to an R0 of about 3. Unfortunately, the CDC places R0 of the Delta variant somewhere between 5 and 9, so vaccination alone is insufficient to control the spread. (As an aside, this also means that given the efficacy estimates for the current vaccines, herd immunity is not possible.)
Next consider the dashed blue line, which represents the stability boundary if we test everyone once per week. If our vaccination rate is greater than about 90 percent, testing one time per week can control even the CDC’s most pessimistic estimate for the Delta variant’s R0.
Q: In returning to campus over the next few weeks, indoor masking and regular testing are required of every MIT community member, even those who are vaccinated. What in your modeling has shown that each of these policies is necessary?
A: Given that the chart above shows that vaccination and weekly testing are sufficient to control the virus, one should certainly ask “Why have we reinstated indoor masking?” The answer is related to the fact that, as a university, our population turns over once a year; every September we bring in a few thousand new people. Those people are coming from all over the world, and some of them may not have had the opportunity to get vaccinated yet. The good news is that MIT Medical has vaccines and will be administering them to any unvaccinated students as soon as they arrive; the bad news is that, as we all know, it takes three to five weeks for resistance to build up, depending on the vaccine. This means that we should think of August and September as a transition period during which the vaccination rates may fluctuate as new people arrive.
The other revelation that has informed our policies for September is the recent report from the CDC that infected vaccinated people carry roughly the same viral load as unvaccinated infected people. This suggests that vaccinated people — although they are highly unlikely to get seriously ill — are a consequential part of the transmission chain and can pass the virus along to others. So, in order to avoid giving the virus to people who are not yet fully vaccinated during the transition period, we all need to exercise a little extra care to give the newly vaccinated time for their immune systems to ramp up.
Q: As the fall progresses, what signs are you looking for that might shift decisions on masking and testing on campus?
A: Eventually we will have to shift responsibility toward individuals rather than institutions, and allow people to make decisions about masks and testing based on their own risk tolerance. The success of the vaccines in suppressing severe illness will enable us to shift to a position in which our objective is not necessarily to control the spread of the virus, but rather to reduce the risk of serious outcomes to an acceptable level. There are many people who believe we need to make this adjustment and wean ourselves off pandemic living. They are right; we cannot continue like this forever. However, we have not played all our cards yet, and, in my opinion, we need to carefully consider what’s left in our hand before we abdicate institutional responsibility.
The final ace we have to play is vaccinating kids. It is important to remember that we have many people in our community with kids who are too young to be vaccinated and, understandably, those parents do not want to bring Covid home to their children. Furthermore, our campus is not just a workplace; it is also home to thousands of people, some of whom have children living in our residences or attending an MIT childcare center. Given that context, and the high probability that a vaccine will be approved for children in the near future, it is my belief that our community has the empathy and fortitude to try to keep the virus in check until parents have the option to protect their children with vaccines.
Bearing in mind that children constitute an unprotected portion of our population, let me return to the original question and speculate on the fate of masks and testing in the fall. Regarding testing, the analysis suggests that we cannot give that up entirely if we would like to control the spread of the virus. Second, control of the virus is not the only benefit we get from testing. It also gives us situational awareness, serves as an early warning beacon, and provides information that individual members of the community can use as they make decisions about their own risk budget. Personally, I’ve been testing for a year now and I find it easy and reassuring. Honestly, it’s nice to know that I’m Covid-free before I see friends (outside!) or go home to my family.
Regarding masks, there is always uncertainty around whether a new variant will arise or whether vaccine efficacy will fade, but, given the current parameters and our analysis, my hope is that we will be in a position to provide some relief on the mask mandate once the incoming members of our population have been fully vaccinated. I also suspect that whenever the mask mandate is lifted, masks are not likely to go away. There are certainly situations in which I will continue to wear a mask regardless of the mandate, and many in our community will continue to feel safer wearing masks even when they are not required.
I believe that we are a generous community and that we will be willing to take precautions to help keep each other healthy. The students who were on campus last year did an outstanding job, and they have given me a tremendous amount of faith that we can be considerate and good to one another even in extremely trying times.