Delivering life-saving oxygen
At the peak of the Covid-19 outbreak in Italy, doctors and healthcare professionals were faced with harrowing decisions. Hospitals were running out of ventilators, forcing doctors to choose which patients had the best chance of survival, and which didn’t.
“It was a very difficult time for Italy,” recalls Daniele Vivona, a mechanical engineering graduate student from Italy. In early March, Vivona and a team of researchers at MIT’s Electrochemical Energy Lab (EEL) started to devise a plan to develop an oxygen concentrator that might one day help hospitals, like those in Italy, deliver oxygen to patients who so desperately need it.
“Traditionally our lab uses electrons to break molecules that generate energy carriers,” explains Yang Shao-Horn, professor of mechanical engineering and EEL’s director. “We wanted to figure out how to take our expertise in electrochemistry and use it to create a device to make an oxygen concentrator that can be delivered to patients.”
Shao-Horn’s team is one of several groups that have been developing technologies to help hospitals around the world provide life-saving oxygen to patients with Covid-19 and other respiratory illnesses.
A low-cost portable oxygen concentrator
As a starting point, Shao-Horn and her team at EEL reached out to Boston-area doctors, as well as doctors in Italy and South Korea, to better understand their needs. They set out to make a low-cost and portable oxygen concentrator to improve clinical management in hospitals that were overwhelmed with Covid-19 patients, in addition to providing solutions that could be adopted in places with limited infrastructure like field hospitals or developing countries.
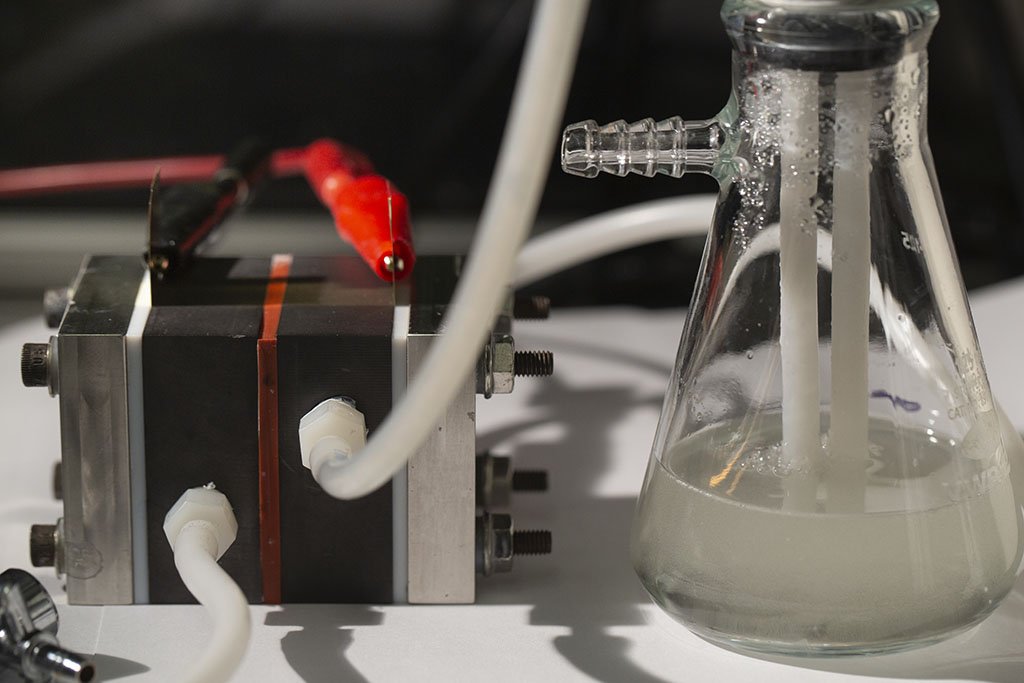
The resulting device resembles a typical electrochemical cell battery. Water and air are pumped through a cell with a cathode that produces negative electrons. The water is passed through a catalytic H2O2 membrane that helps separate oxygen from the air before being positively charged by an anode. After passing through an oxygen compressor, pure oxygen then flows to an oxygen tank, where it can be readily delivered and used to treat patients.
Postdoctoral associate C. John Eom has been leading efforts to improve the cathode and anode in the device, while fellow postdoctoral associate Yunguang Zhu has been focusing on the chemistry involved in the H2O2 membrane.
As the team continues to work on the concentrator, they are looking into various ways it can help doctors save lives – including while transporting patients from the ICU to the operating room.
“We’re hoping to have something portable enough that patients could potentially use the device at home and we provide doctors with more options to address diverse situations that require the delivery of oxygen to patients,” says Eom.
Open-source ventilator designs
Stories of Italian hospitals running out of ventilators were the impetus for another MIT-led project known as the MIT Emergency Ventilator Team. “This project started around the time of news reports from Italy describing ventilators being rationed due to shortages, and available data at that time suggested about 10 percent of Covid patients would require an ICU,” alum Alexander Slocum Jr. SB ’08, SM ’10, PhD ’13 told MIT News in April.
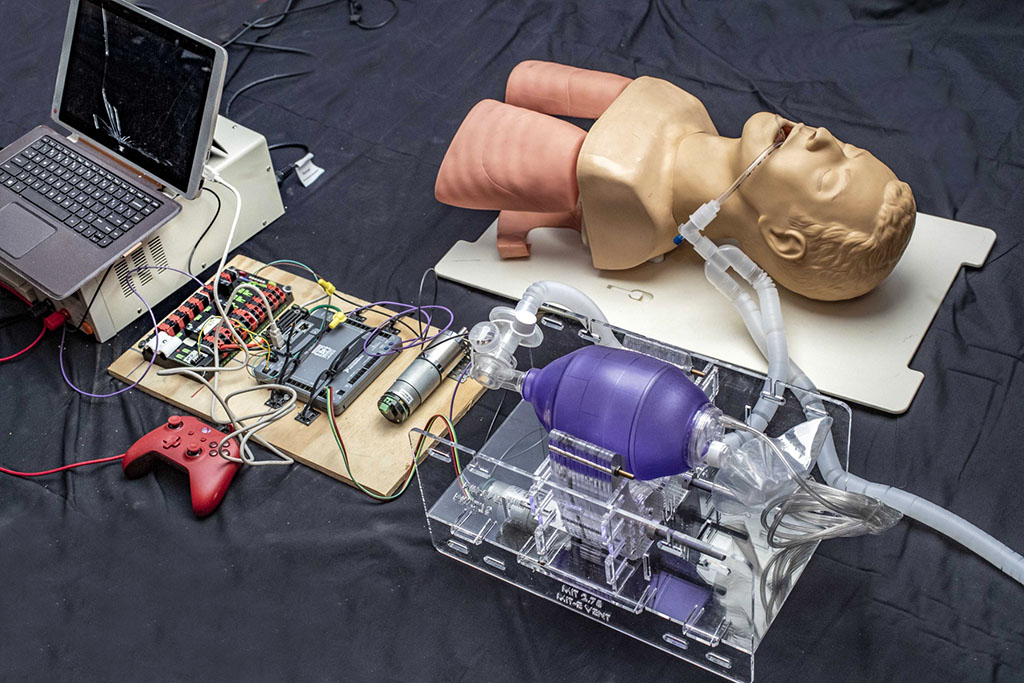
Slocum Jr. worked with his father Alexander Slocum Sr., Walter M. May and A. Hazel May Professor of Mechanical Engineering, as well as research scientist Nevan Hanumara SM ’06, PhD ’12, and together they developed a plan to release an open- source design that companies worldwide could then use to manufacture low-cost ventilators for emergency use.
“We realized that as researchers, our best role would be supporting other people who had more capabilities to execute and produce ventilators than we did,” recalls Hanumara. “So, we focused heavily on developing the base requirements for safe low-cost ventilation and, following from this, a reference hardware and software design.”
The team grew to include MIT graduate students and alumni, including a trio from Professor Daniela Rus’s group in MIT CSAIL. They used a design developed in the mechanical engineering class 2.75, Medical Device Design, back in 2010 as a starting point. Graduate student Kimberly Jung, a West Point graduate who has served in the Army, acted as the “executive officer,” holding the team together.
With insights gathered from the clinical community, they developed multiple prototype iterations, wrote code, and conducted animal studies. As the work progressed, it was posted to an opensource site. Within a few months, over 24,000 people had registered to gain access to the site.
“Since March there has been a tremendous and humbling international response to our work,” adds Hanumara. The team has refocused to help groups around the world refine the designs and deploy ventilators. From an all-girl robotics team in Afghanistan to groups in New York, Ireland, India, Chile, and Morocco, Hanumara and the MIT Emergency Ventilator team have been helping others develop solutions that fit their own country’s needs.
Splitting ventilators to treat multiple patients
Giovanni Traverso, Karl Van Tassel (1925) Career Development Professor of Mechanical Engineering, together with collaborators from Brigham and Women’s Hospital, Massachusetts General Hospital, and Philips, took a different approach in trying to solve the ventilator shortage. Their effort, led by postdoctoral associate Shriya Srinivasan PhD ’20, developed a method to split a ventilator so it can treat two or potentially more patients at a time instead of one. Their approach is meant only as a last resort when there aren’t enough ventilators to meet the need.
“We saw this as an opportunity where we might be able to help hospitals facing ventilator shortages due to Covid-19,” says Traverso. “While other teams were developing new ventilators, our approach was to address situations where people can’t make their own ventilators or augment the capacity of all ventilators. We wanted to help inform how they could amplify their current capacity further.”
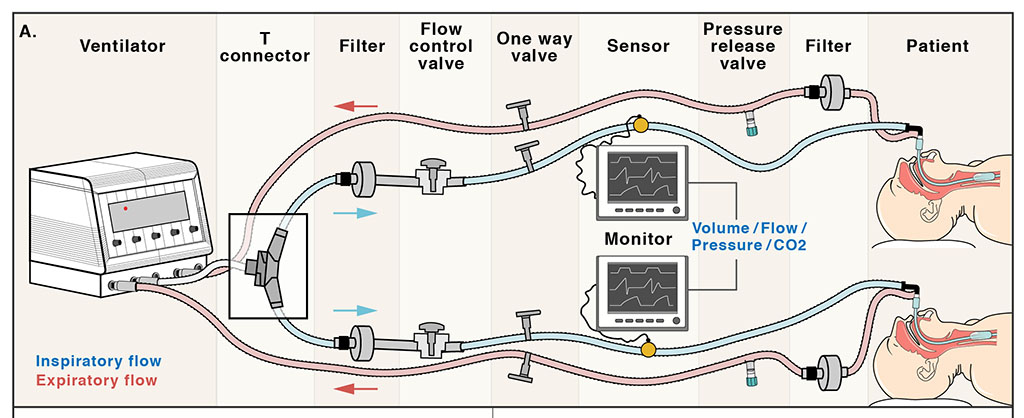
Splitting ventilators between two patients provides a host of logistical issues including matching flow rates and delivering the same amount of oxygen to two patients who may have different needs. “Previous designs haven’t provided the ability to customize the treatment to each patient, who will invariably present with variable needs,” says Srinivasan. “Our approach focused closely on this aspect and enabled the customization of volume and pressure for each patient.”
“We knew splitting ventilators was a major challenge, so we aimed to understand what the challenges were and address them to make it feasible to treat multiple patients using one ventilator,” adds Traverso
To tackle these challenges, Srinivasan and Traverso added two flow valves to the split ventilator. Healthcare professionals can use these valves to tailor the flow of oxygen to each individual patient. The team also added new safety measures, including pressure release valves and alarms, to make sure patients don’t receive too much or too little oxygen as their condition changes.
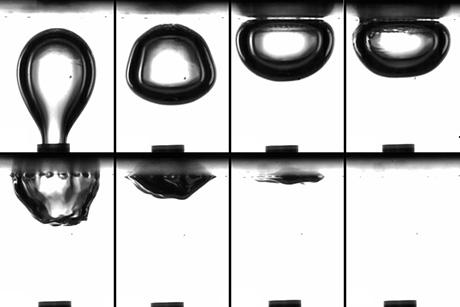
The research team was able to successfully test their new method with the help of an artificial lung and through simultaneous ventilation of two pigs. As with the MIT Emergency Ventilator Team, the team is working with international groups to bring the split ventilator technology to countries that need additional infrastructure to treat patients with respiratory diseases like Covid-19. Their research was published in Science Translational Medicine and the team started a non-profit, Project Prana, to help support the dissemination of the work.
“We’re also working with large healthcare systems and startups in India, Bangladesh, and Venezuela to bring the system to the rural towns that have run out of ventilators and cannot afford emergency ventilators,” Srinivasan says.
While the methods were different, these three research teams share a central purpose: to provide oxygen to those whose lives depend on it. Whether it’s through electrochemical reactions, open-source ventilator designs, or splitting ventilators, this research could help hospitals weather further spikes in Covid-19 cases and put solutions in place in the event of future pandemics.